One of my joys in being spatial with birth observation skills is being asked to be a “Birth Detective”. Parents often want to know why a previous birth was difficult. Here’s a woman planning for a vaginal birth after a previous cesarean (VBAC). What can you identify as potential issues and potential solutions which her doctor or midwife might seek for a vaginal birth this time? This response is edited for privacy.
“I am 33 weeks pregnant with my second child, and am attempting a VBAC. My first child was consistently posterior and almost always on my right side. After a 47 1/2 hour labor (that included 6 hours of pushing), we ended up with a c-section after reaching +2. It was discouraging to say the least!
Now, my second pregnancy seems to be following the same path. The baby is almost always posterior on my right, or down the center. I have been implementing:
I have been doing everything I know to do to prepare for my VBAC and try to prevent another c-section. I am very concerned about this baby not being left anterior and my birth ending up in another c-section! My midwife is very experienced (over 30 years of experience) … She does not seem to be very familiar with Spinning Babies® and when I stressed my concern to her, she responded by telling me that she has birthed many posterior babies and that she is confident my birth will be successful. My doula is familiar with Spinning Babies.
I am concerned that while I am doing everything I can to implement Spinning Babies knowledge and get the baby properly positioned, that my birth attendants will not be able to help me if my baby doesn’t change sides. I purchased the Spinning Babies® Parent Class. Should I ask my doula to take a look at it? And what your advice be to me?”
Of course, an online source (even myself), is no substitute for her provider. Hands-on assessment can prevent assumption. The trouble is, the usual way of supporting VBAC is with time and usual positions. The skills that a 30-year midwife has in supporting a VBAC are immense. Yet the knowledge Spinning Babies® brings in for addressing the anatomy of both the soft tissue and bony pelvis goes beyond the knowledge base of midwifery. Combining both knowledge bases adds resourcefulness for VBAC care; homebirth midwifery with Spinning Babies perspective (which arises from my observations at home births, hospital births, and published research analysis).
This brave and bold woman’s description gives a clear clue as to a likely cause for the lack of progress in her first birth. [Is she brave and bold if birth is normal? Then her desire and work towards a vaginal birth is normal… What’s brave about that? EVERYTHING! I celebrate the Birth Giver. I celebrate a person who digs in deep and seeks the expression of what can be!]
Put on your birth detective hat and see if you can find the “Spinning Babies® view”. Use your knowledge of the 3 Levels of the Pelvis from the early lessons in these emails or your Spinning Babies® Workshop or The Spinning Babies® Quick Reference (A Trainer in your pocket!)
It has to do with the station, or level, of the pelvis where baby waited. Do you see it? +2.
What do we know about +2.
Baby engaged! Baby made it lower than the ischial spines!
+2 is low enough to consider outlet but the baby is not visible. Let’s back up a bit then. Baby isn’t quite coming to the outlet… Most techniques for the outlet also help +2 which borders the midpelvis and outlet.
What can we know that may help this woman express her full physiology?
Anatomically, the first baby has navigated the midpelvis.
At +2, baby is passing the rami on the sides and the sacrum in the back. These bony structures are usually quite wide and mobile for baby. When progress stops here, there may be a few reasons why:
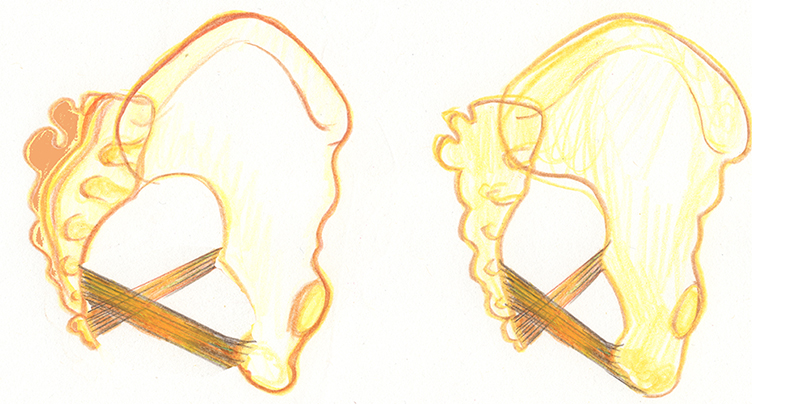
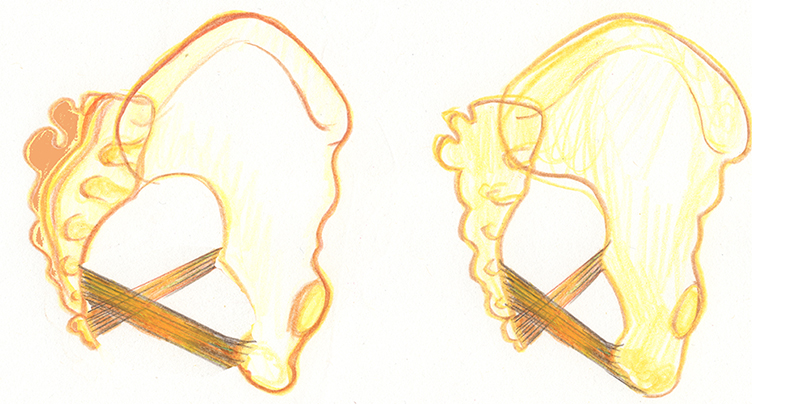
Or, the sacrum is locked and too close to one or both of the sitz bones. See drawing. In this case, no full-term baby is coming out, regardless of position. “The baby won’t come until the back opens” say the Jamaican midwives and this “back” can’t open – yet!
What can we offer? Look in your inbox next week to read our suggested activities for preventing another labor dystocia at +2 Station. This week, consider what would you do with the above information to support VBAC. Drop us a comment on our Facebook post for today.
[tribe_events_list limit=”4″]