 What is a posterior fetal presentation? The baby’s back is spine-to-spine with the mother.
What is a posterior fetal presentation? The baby’s back is spine-to-spine with the mother.
Why would posterior position matter in labor? The head is angled so that it measures larger. The top of the head molds less than the crown.
Baby’s spine is extended, not curled, so the crown of the head is not leading the way. Baby can’t help as much during the birth process to the same degree as the curled up baby.
Some posteriors are easy, while others are long and painful, and there are several ways to tell how your labor will be beforehand. After this, you may want to visit What to do when….in Labor.
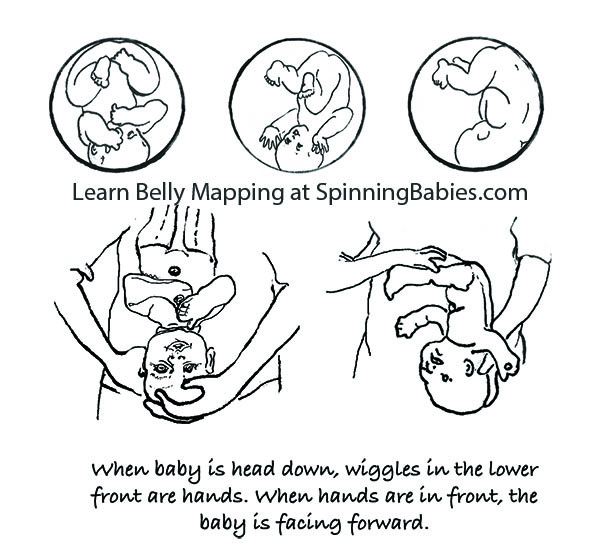
Belly Mapping® Method tips: The Right side of the abdomen is almost always firmer, but the direct OP baby may not favor one side or the other. Baby’s limbs are felt in front, on both sides of the center line. A knee may slide past under the navel.

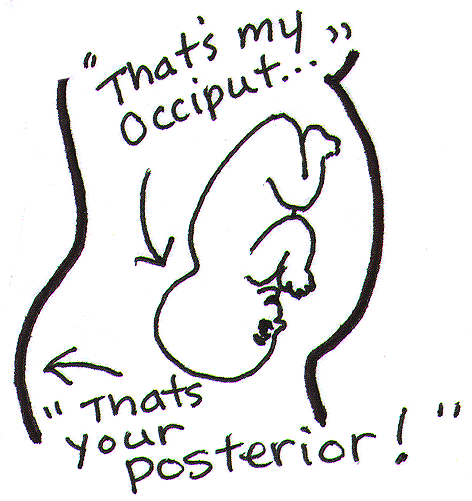
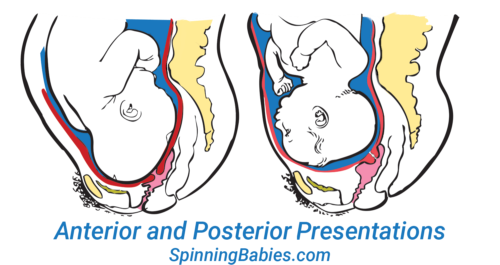
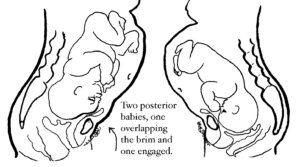
The OP position (occiput posterior fetal position) is when the back of the baby’s head is against the mother’s back. Here are drawings of an anterior and posterior presentation.

Look at the above drawing. The posterior baby’s back is often extended straight or arched along the mother’s spine. Having the baby’s back extended often pushes the baby’s chin up.
Attention: Having the chin up is what makes the posterior baby’s head seem larger than the same baby when it’s in the anterior position.
Because the top of the head enters (or tries to enter) the pelvis first, baby seems much bigger by the mother’s measurements. A posterior head circumference measures larger than the anterior head circumference.
A large baby is not the same issue, however. The challenge with a posterior labor is that the top of the head, not the crown of the head leads the way.
A baby with their spine straight has less ability to wiggle and so the person giving birth has to do the work of two. This can be long and challenging or fast and furious. Also, there are a few posterior labors that are not perceived different than a labor with a baby curled on the left.
Why? Anatomy makes the difference. Learn to work with birth anatomy to reduce the challenge of posterior labor by preparing with our Three BalancesSM and more.
What to do?
In Labor, do the above and add,
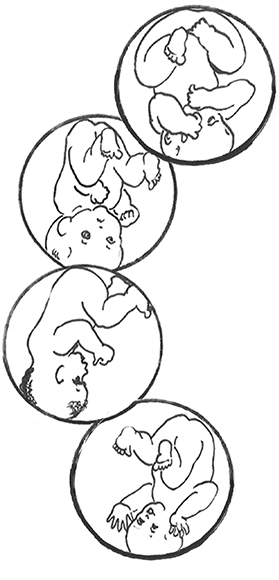
The direct OP is the classic posterior position with the baby facing straight forward. Right Occiput Transverse (ROT) is a common starting position in which the baby has a bit more likelihood of rotating to the posterior during labor than to the anterior. Right Occiput Posterior usually involves a straight back with a lifted chin (in the first-time mother). Left Occiput Posterior places the baby’s back opposite the maternal liver and may let the baby flex (curl) his or her back and therefore tuck the chin for a better birth. These are generalities, of course. See a bit more about posterior positions in Belly Mapping® on this website. Want to map your baby’s position? Learn how with the Belly Mapping® Workbook.
Pregnancy may or may not show symptoms. Just because a woman’s back doesn’t hurt in pregnancy doesn’t mean the baby is not posterior. Just because a woman is quite comfortable in pregnancy doesn’t mean the baby is not posterior. A woman can’t always feel the baby’s limbs moving in front to tell if the baby is facing the front.
Four starting positions often lead to (or remain as) direct OP in active labor. Right Occiput Transverse (ROT), Right Occiput Posterior (ROP), and Left Occiput Posterior (LOP) join direct OP in adding labor time. The LOP baby has less distance to travel to get into an LOT position.
As labor begins, the high-riding, unengaged Right Occiput Transverse baby slowly rotates to ROA, working past the sacral promontory at the base of the spine before swinging around to LOT to engage in the pelvis. Most babies go on to OA at the pelvic floor or further down on the perineal floor.
If a baby engages as a ROT, they may go to OP or ROA by the time they descend to the midpelvis. The OP baby may stay OP. For some, once the head is lower than the bones and the head is visible at the perineum, the baby rotates and helpers may see the baby’s head turn then! These babies finish in the ROA or OA positions.
Feeling both hands in front, in two separate but low places on the abdomen, indicates a posterior fetal position. This baby is Left Occiput Posterior.
Studies estimate 15-30% of babies are OP in labor. Jean Sutton in Optimal Fetal Positioning states that 50% of babies trend toward posterior in early labor upon admission to the hospital. Strong latent labor swings about a third of these to LOT before dilation begins (in “pre-labor” or “false labor”).
Recent research shows about 50% of babies are in a posterior position when active labor begins, but of these, 3/4 of them rotate to anterior (or facing a hip in an occiput transverse, head down position.
Jean Sutton’s observations, reported in her 1996 book, indicates that some babies starting in a posterior position will rotate before arriving to the hospital. Ellice Lieberman observed most posteriors will rotate out of posterior into either anterior or to facing a hip throughout labor. Only 5-8% of all babies emerge directly OP (13% with an epidural in Lieberman’s study). At least 12% of all cesareans are for OP babies that are stuck due to the larger diameter of the OP head in comparison to the OA head. It’s more common for ROT, ROP, and OP babies to rotate during labor and to emerge facing back (OA). Some babies become stuck halfway through a long-arc rotation and some will need a cesarean anyway.
 The three anteriors — LOT, LOA, and OA — are all ideal fetal positions for the start of labor. Both LOA and OA require less rotation than LOT and may lead to a faster labor, but they may also be less common. Generally, very few midwives or doctors will pay strict attention to the actual head position, leading to the LOT baby often being referred to as LOA or just OA.
The three anteriors — LOT, LOA, and OA — are all ideal fetal positions for the start of labor. Both LOA and OA require less rotation than LOT and may lead to a faster labor, but they may also be less common. Generally, very few midwives or doctors will pay strict attention to the actual head position, leading to the LOT baby often being referred to as LOA or just OA.
Why not ROA? ROA babies may have their chins up and this deflexed position may lengthen the course of labor. Less than 4% of starting positions are ROA, according to a Birmingham study. This might not be ideal for first babies, but is not a posterior position either.

There is a spectrum of ease across posterior labors. It’s not a bell curve, though; easy posteriors are not as common as challenging ones. Usually, babies turn after many strong contractions. Without help, almost half of women will give birth to their posterior babies. The techniques called The Fantastic Four are likely to improve mothers’ and babies’ ease of birth! Learn these techniques that will help you avoid unnecessary surgery for your baby’s birth by watching the Spinning Babies® Parent Class video:
With a posterior presentation, labor may or may not be significantly affected. There is a spectrum of possibilities with a posterior baby. Some women will not know they had a posterior baby because no one mentions it. Either the providers didn’t know, or didn’t notice. If labor moved along, they may not have looked at fetal position clues since there was no reason to figure out why labor wasn’t progressing. If a woman didn’t have back labor (more pain in her back than in her abdomen), the provider may not have been “clued into” baby’s position.
Some posterior babies are born in less than 8 hours and position did not slow down labor. Some posterior babies are born in less than 24 hours and position did not slow down labor enough to be out of the norm. Some posterior babies are born in less than 36-48 hours without the need for interventions.
Some posterior labors are manageable when women are mobile, supported, and eat and drink freely, as needed. Some posterior labor needs extra support that a well-trained and experienced doula may provide, but that typically a mate or loved one would not have the skills or stamina to keep up with. Some posterior labors progress only with the help of a highly-trained pregnancy bodyworker or deep spiritual, or otherwise a non-conventional model of care. Or, they seem only able to finish with medical intervention.
Some posterior labors are served by an epidural, meaning the pelvic floor relaxes enough for the baby to rotate and come out. Some epidurals, on the other hand, make it so that a woman can not finish the birth vaginally.
NOTE: Parents should know — some birth researchers, like Pediatrician John Kennell, are seriously asking whether a mother’s epidural turns off her body’s release of pain-relieving hormones which a baby relies on during childbirth. Some babies can’t turn and can’t be born vaginally and must be born by cesarean. This is a spectrum of possibilities. I’ve seen every one of the above possibilities several times and can add the wonderful experience of seeing a woman laughing pleasurably and squatting while her posterior baby slid out on to her bedroom floor.

These effects are in comparison to a baby in the left occiput anterior or left occiput transverse fetal position at the start of labor.
Who is likely to have an easy time with a posterior baby?
Any woman may also have an easier time than public opinion might indicate, too, just because she isn’t on this list. Equally, just because she is on the “hard” list doesn’t mean she will have a hard time for sure. These are general observations. They are neither condemnations nor promises. Overall, some posterior babies will need help getting born, while some posterior babies are born easily (easy being a relative term).
While most posterior babies do eventually rotate, that can still mean there is quite a long wait – and a lot of physical labor during that wait. Sometimes it means the doula, midwife, nurse, or doctor is asking the mother to do a variety of position changes, techniques, and even medical interventions to help finish the labor. Patience works for many, but for some a cesarean is really the only way to be born. Read What To Do When…in Labor.
There is a rising incidence of posterior babies at the time of birth. We know now that epidural anesthesia increases the rate of posterior position at the time of birth from about 4% (for women who don’t choose an epidural in a university birth setting) up to about 13% (Lieberman, 2005). Low thyroid function is associated with fetal malposition such as posterior or breech. (See Research & References.)
Most babies who are posterior early in labor will rotate to anterior once labor gets going. Some babies rotate late in labor, even just before emerging. Studies such as Lieberman’s show that at any given phase of labor, another 20% of posterior babies will rotate so that only a small number are still posterior as the head emerges.
My observations are that the majority of babies are posterior before labor. The high numbers of posterior babies at the end of pregnancy and in the early phase of labor is a change from what was seen in studies over ten years old. Perhaps this is from our cultural habits of sitting at desks, sitting in bucket seats (cars), and leaning back on the couch (slouching). Soft tissues such as the psoas muscle pair or the broad ligament also seem to be tight more often from these postures, from athletics (quick stops, jolts, and falls), from accidents, and from emotional or sexual assault.
Being a nurse or bodyworker who turns to care for people in a bed or on a table will also twist the lower uterine segment (along with some of the previously mentioned causes). This makes the baby have to compensate in a womb that is no longer symmetrical. Less often, the growing baby settles face-forward over a smaller pelvis, or a triangular-shaped pelvis (android). At the end of pregnancy, the baby’s forehead has settled onto a narrower than usual pubic bone, and if tight round ligaments hold the forehead there, the baby may have a tough time rotating. These are the moms and babies that I’m most concerned with in my work at Spinning Babies®. A baby that was breech beyond week 30 – 34 of pregnancy will flip head down in the posterior position. A woman with a history of breech or posterior babies is more likely to have a breech or posterior baby in the next pregnancy. However, she may not have an as long labor.
The best way to tell if your baby is OP or not, usually, is if you feel little wiggles in the abdomen right above your pubic bone. These are the fingers. They’d feel like little fingers wiggling, not like a big thunk or grinding from the head, though you might feel that, too. The little fingers will be playing by the mouth. This is the easiest indication of OP. The wiggles will be centered in the middle of your lower abdomen, close to the pubic bone. If you feel wiggles far to the right, near your hip, and kicks above on the right, but not near the center and none on the left, then those signal an OA or LOT baby (who will rotate to the OA easily in an active birth). After this, you might go to What to do when…in Labor.
Check out our current references in the Research & References section.
For additional education to even further enhance your pregnancy and labor preparation, shop our extensive collection of digital downloads, videos, DVDs, workbooks, and more.