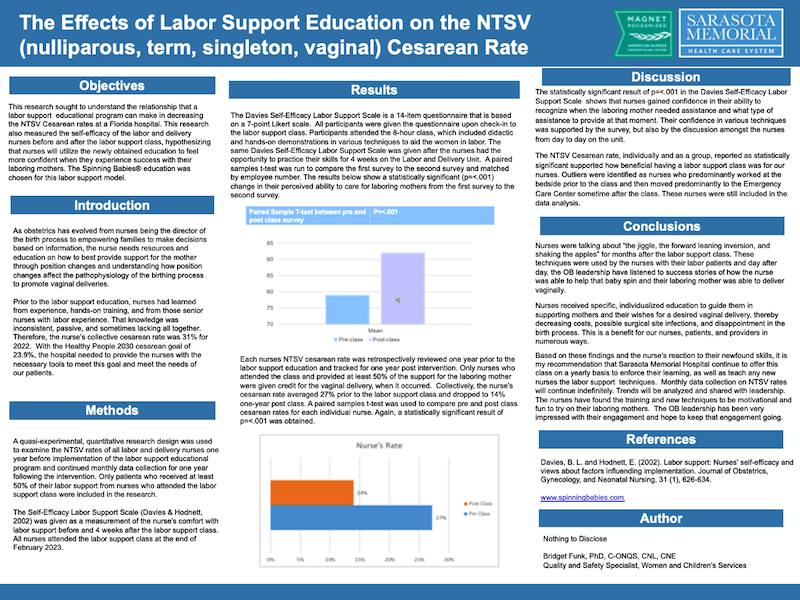
This clinical trial highlights the effectiveness of Spinning Babies® techniques in reducing cesarean rates, particularly for nulliparous, term, singleton, vaginal (NTSV) births. The results show that after nurses received Spinning Babies® training, the cesarean rate decreased from 27% to 14% in the hospital where the training was implemented. This significant decrease demonstrates the power of body balancing and physiological labor support in reducing unnecessary interventions.
In addition to the cesarean reduction, nurses trained in Spinning Babies® showed a statistically significant improvement in their ability to support laboring mothers naturally, without relying on interventions. This boost in confidence was reflected in their hands-on work with laboring mothers and their ability to assist in facilitating fetal descent.
The study also included a review of each nurse’s NTSV cesarean rate over one year before the training, revealing clear improvements in cesarean rates following the education. This emphasizes the lasting impact of Spinning Babies® methods in transforming labor outcomes. Statistically significant results were found after nurses participated in the 8-hour Spinning Babies® workshop, further proving the effectiveness of the techniques.
Nurses reported increased confidence in assisting with labor, especially in reducing the need for interventions and helping babies move through the pelvis. The study underscores the value of empowering healthcare providers with effective, physiological labor support practices that result in better birth outcomes for both mothers and babies.
Funk, B. (2024). The Effects of Spinning Babies® on the Nulliparous, Term, Singleton, Vertex Cesarean Rates. Journal of Obstetric, Gynecologic & Neonatal Nursing, 53(4), S83.
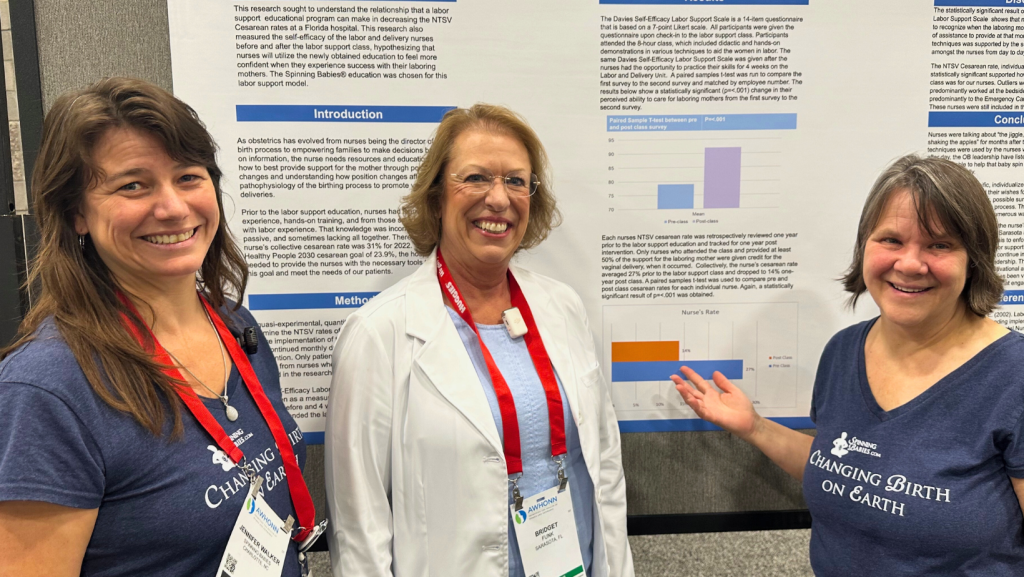
Bridget Funk, RN, shares the results of using Spinning Babies® approach in her hospital, Sarasota Memorial at the 2024 AWHONN National Convention. Workshop given by Spinning Babies® Approved Trainer, Kelly Dungan.
A 2025 study out of Italy demonstrates that Spinning Babies® helps posterior babies rotate! “The use of the Spinning Babies® techniques was associated with a 45% increased likelihood of achieving anterior position.” Learn more here.
This study highlights the effectiveness of Spinning Babies® techniques in reducing cesarean rates, particularly for nulliparous, term, singleton, vaginal (NTSV) births. The results show that after nurses received Spinning Babies® training, the cesarean rate decreased from 27% to 14% in the hospital where the training was implemented. This significant decrease demonstrates the power of body balancing and physiological labor support in reducing unnecessary interventions.
In addition to the cesarean reduction, nurses trained in Spinning Babies® showed a statistically significant improvement in their ability to support laboring mothers naturally, without relying on interventions. This boost in confidence was reflected in their hands-on work with laboring mothers and their ability to assist in facilitating fetal descent.
The study also included a review of each nurse’s NTSV cesarean rate over one year before the training, revealing clear improvements in cesarean rates following the education. This emphasizes the lasting impact of Spinning Babies® methods in transforming labor outcomes. Statistically significant results were found after nurses participated in the 8-hour Spinning Babies® workshop, further proving the effectiveness of the techniques.
Nurses reported increased confidence in assisting with labor, especially in reducing the need for interventions and helping babies move through the pelvis. The study underscores the value of empowering healthcare providers with effective, physiological labor support practices that result in better birth outcomes for both mothers and babies.
This publication details how Spinning Babies® supports professional development and the reduction of cesarean rates in a Florida hospital with extremely high cesarean rates.
This study looked at use of Spinning Babies® as a physiological support for birthing women of “racial and ethnic minorities”. Women with more challenging births had less satisfaction compared to women who didn’t rate their births as complicated; but other than such complicated birth, birth satisfaction didn’t seem to vary by race when supported with the Spinning Babies® approach. The use of our approach could be one intriguing way to equalize and promote physiological birth care among communities in the United States.
12 Midwives give qualitative reports on their experience with Spinning Babies®.
This study discusses the role of evidence-based practice in reducing cesarean rates, relevant to how Spinning Babies® techniques can play a role in that process. Learn more here
This research includes a partial application of concepts that Spinning Babies® propose in our approach. There will be a mention of Spinning Babies® but these are not research ON Spinning Babies®.
This publication details how Spinning Babies® supports professional development and the reduction of cesarean rates in a Florida hospital with extremely high cesarean rates. This is actually the same report as Euda, below.
In Park’s pilot project nurses used a variety of comfort measures including techniques shared through Spinning Babies®. Gail Tully’s “Spinning Babies book” is cited, and very likely that book is Changing Birth on Earth, a book written for the Intrapartum nurse and midwife, since that was the main book available at the time this article was published.
Ariana Parkhideh uses interviews and surveys to understand the perspectives of doulas on the Black maternal health crisis and the strategies they use to support clients. “Both Joy and Renie incorporate Spinning Babies®, a series of positioning, massage [massage isn’t actually a part of our approach though it’s lovely], and other techniques to facilitate easier childbirth by balancing the pelvis and potentially repositioning the fetus, into the services they provide to her birth clients… ”
Thank you, Joy and Renie, we are truly grateful to be included through your doula care to reduce violence against birth people and to be able to have something positive to offer Black Maternity.
This is definitely not a study on Spinning Babies® but most nurses in this hospital were familiar with Spinning Babies®. Ueda interviewed nurses and asked what their confidence was with birth positions. “53.5% (n=23) of nurses had additional off-unit training for labor positions such as Spinning Babies®” Just less than half had no training in physiologic birth positions. The birth position posters shown the nurses to inspire position changes did not include Spinning Babies® recommended positions nor did they use our labor progress tracking approach. But it is important to note that half their staff was given at least one day of Spinning Babies® training. It is proposable to suggest that their project conclusions included a higher confidence in birth positioning with the added knowledge base that over half of their nurses had from self-obtained study with Spinning Babies®. They suggest that “The results of this project show that standardization of these labor positions is the next step to improving patient outcomes.” It would be wonderful to have Spinning Babies® birth positions poster inform more hospitals before assuming that birth positions are as basic as upright, on the back, or on the side.
This study on fetal “starting” positions at the onset of labor or during the various phases of labor highly supports Gail Tully’s proposals. This study, however, is researching the effectiveness of the length of labor and outcomes that Jean Sutton talks about in Optimal Fetal Positioning.
Witkiewicz found: The distribution of individual initial positions of the head in the right foetal position was as follows: ROP 45.1%, ROT 35.4%, ROA 6.15%, and a position difficult to determine 13.35%. In the left position, it was as follows: LOA 28.6%, LOT 57.1%, LOP 4.3%, and a position difficult to determine 10%. And while LOA is often cited as Jean Sutton’s single optimal position, she said, and if you read all her material completely you’ll find it, that the left side is optimal, even rather the LOP. Spinning Babies® has based much emphasis on Jean Sutton’s affirmation that easier birth when baby begins on the left (which was first in 1800’s medical literature) and that VERY OFTEN But NOT ALWAYS a labor is more challenging when babies start labor on the right side before or at the time of engagement. Gail disagrees with Barth’s proposal not to take any measures to ease the ROP labor for those with a deeper AP inlet measurement. We propose “body balancing” for “all” and especially for those with a baby remaining on the right side, as well as other indicators, no matter inlet or pelvic shape, rather than a “wait and see” approach. We deeply appreciate the words of the authors to de-pathologize labors with babies on the right side of the uterus and emphasizing that physiology persists with any fetal position. That said, we take note when baby persists on the right side, whether in late pregnancy, labor onset, or any time during labor. We take note, we follow invitations to attend to physiology, but we don’t blame, shame, or defame us human beings or our birth process.
This article does not discuss recommendations of what to do and calls for more research (see studies in Section A. Research on Spinning Babies®).
Congratulations to this research team for a very comprehensive observational report!